
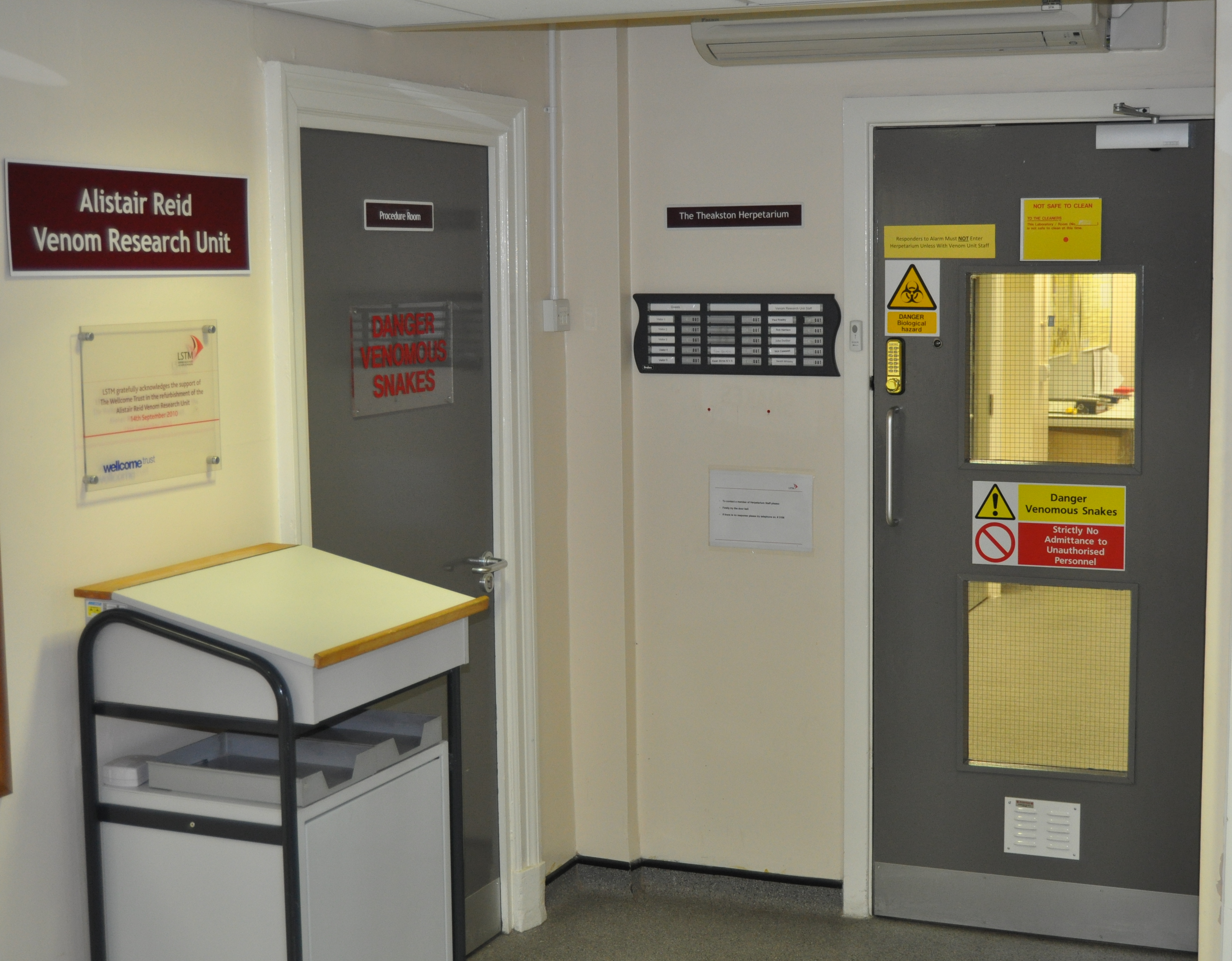
The Alistair Reid Venom Research Unit (ARVRU) conducts a diverse portfolio of research activity to guide research for improving the efficacy, safety and affordability of treatment of tropical snakebite victims. The Herpetarium houses Europe’s largest and most diverse academic collection of venomous snakes. largest collection of venomous snakes in the UK, for use in clinical and scientific studies

The Alistair Reid Venom Research Unit has several current research themes and activities
1) Development of next generation snakebite therapies and diagnostics:
Current anti-venom treatment is weakly effective, induces high levels of adverse effects and is ineffective against the tissue-destructive effects of venom. To significantly improve snakebite treatment, and with an African-focus, we are pioneering the exploitation of modern technical platforms (venom transcriptomics, proteomics and genomics) to develop snakebite therapies with continent-wide efficacy, irrespective of the causative venomous snake species or the variant haemorrhagic, coagulopathic or neurotoxic effects of their venoms.
Furthermore, since antivenom is snake species specific, treatment is often inaccurate or delayed due to the absence of rapid diagnostic tools. We therefore also aim to develop a rapid, affordable, diagnostic test as an urgently needed clinical tool to improve the accuracy and rapidity of antivenom treatment.
3) The ARVRU also has a strong record of undertaking basic biological research (for a list of our publications, see here). Our primary focus is basic research on the evolution, toxicity-control and composition of the venom system of snakes. We have significantly contributed to advocacy campaigns aimed at reversing the government and International Health Agency neglect of tropical snakebite victims, with frequent appearances in the media.
4) Developing new tools in response to the growing threat of bacterial diseases. The resistance of multiple bacterial species to current antibiotic treatments is recognised as one of the most serious threats to human health. There is an urgent need to respond to this threat with research designing rapidly effective therapeutic innovations for translation into point of care products. Prior to discovery of the polyspecific efficacy of antibiotics, serotherapy was the primary treatment of bacterial diseases. Serotherapy (antivenom) remains the primary treatment of snakebite and can be rapidly effective at reversing haemotoxic and neurotoxic pathologies. We have pioneered a novel epitope-string immunogen approach to developing polyspecific serotherapy that neutralises the multiple protein threats posed by snake envenoming. We now seek to use this approach to develop a serotherapy for (i) bacterial necrotising fasciitis - limb amputation is frequently required because current treatment is insufficiently rapid, and (ii) as a secondary line of treatment in vulnerable patients with anti-microbial resistance.

5) We specifically address areas of snakebite management which have received little or no research attention previously. An example of this is our response to the antivenom crisis in Nigeria: we formed the EchiTab Study Group whose most significant output was the design, testing and delivery (37,000 vials) of 2 new antivenoms for snakebite victims in Nigeria. We are continuing this kind of interventional, in-country activity. Thus, we have designed and are testing, in Kenya, a novel Snakebite Emergency Response Systems (SERS) to mitigate poverty as an impediment to accessing effective healthcare. The SERS project is based upon smartphone app-activation of specially-designed motorcycle ambulances to speed rural, remote snakebite victims to well-equipped and trained health care. We seek to complement the SERS program by establishing a network of Snakebite Intervention and Research Centres (SIRCs) in West, Central and East Africa. We will collate the diverse outputs/lessons learned from pilot clinical, biological and epidemiological research projects in countries that represent the diverse cultures, health infrastructures, habitats and venomous snake species in sub-Saharan Africa. The diverse medical, capacity-strengthening and research-empowering outputs of the SIRC program is designed to institute a sustainable system to reduce snakebite mortality, physical disability and stigmatising disfigurement currently suffered by snakebite victims in sub-Saharan Africa.
